Note: Your progress in watching these videos WILL NOT be tracked. These training videos are the same videos you will experience when you take the full ProPALS Recertification program. You may begin the training for free at any time to start officially tracking your progress toward your certificate of completion.
Atrial fibrillation (also called AFib or AF) is a quivering or irregular heartbeat (arrhythmia) that can lead to blood clots, stroke, heart failure, and other heart-related complications.
In this lesson, we'll look at the three types of atrial fibrillation and then look at a typical ECG readout for a patient in AFib and provide a cardiac interpretation at the end.
The Three Types of Atrial Fibrillation
1. Transient
Transient atrial fibrillation is defined by the following:
- Episodes that stop on their own
- Episodes that last anywhere from seconds to minutes, hours, or even up to one week
2. Persistent
Persistent atrial fibrillation is defined by the following:
- Episodes that last longer than one week
- Episodes that last less than one week but are only stopped using either pharmacological intervention or electrical cardioversion
3. Long-Standing Persistent
Long-standing persistent atrial fibrillation, formerly known as chronic or permanent atrial fibrillation, is defined as episodes that last longer than a year.
Atrial fibrillation occurs when multiple electrical impulses are being generated in the atria and at the same time, which causes chaotic myocardia responses.
AFib can diminish the preload and effectiveness of the cardiac contractions. This action could then cause the development of microemboli due to stagnant blood flow from the atria. In certain instances, this will even lead to a rapid ventricular response that's secondary to a reentry problem.
Pro Tip #1: The electrical pattern on an ECG will have no discernible P-waves, but instead, will show fibrillatory waves between each QRS complex. And because there's a lack of coordinated electrical impulses generated from the atria traveling through the AV node into the ventricles, the result is usually an irregular ventricular response, which also occurs irregularly.
Now let's take a look at an ECG for a patient in atrial fibrillation.
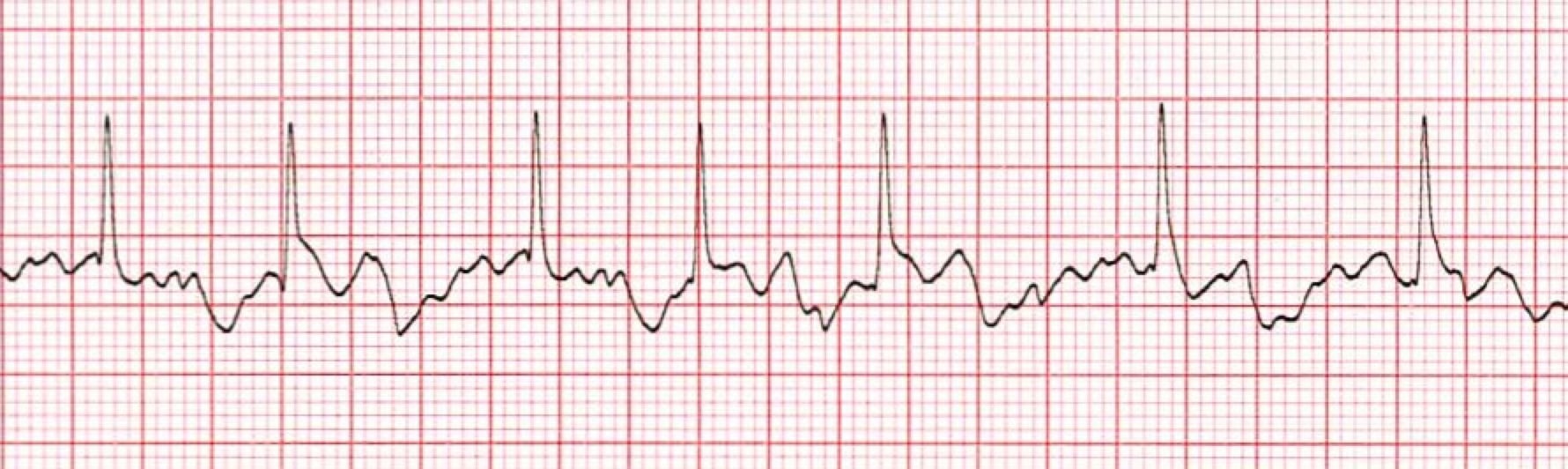
*Atrial Fibrillation ECG
1. The Heart Rhythm
The first thing you'll want to look at is the heart rhythm. Does the heart rhythm look regular? Or does it look irregular? In the ECG above, the rhythm is irregular.
2. The Heart Rate
Next, you'll want to look at the heart rate of the patient. What is the patient's heart rate? Is it normal? Or is it too slow or too fast? In this case, it's 80 beats per minute, but it's also irregular.
3. P-Wave
After looking at the heart rate, check to see if the patient's P-waves look normal by asking yourself the following few questions.
- Are the patient's P-waves present? No!
- Do they occur regularly? The answer is obviously no again.
- Is there one P-wave for each QRS complex? No.
- Are the P-waves smooth, rounded, and upright? No, only fibrillatory waves are present.
- Do all the P-waves have a similar shape? Again, that answer is no, because they aren't present.
4. PR Interval
Next, look at the PR interval on the patient's ECG readout and ask yourself the following questions:
- Is the PR interval normal, meaning less than .20 seconds or is it contained within one large square on the readout? The answer is no, because there isn't a PR interval.
- Is the PR interval constant? Again, this in non-applicable since there isn't a P-wave.
5. QRS Complex
The last thing you should look at to determine if the sinus rhythm is normal or not is the QRS complex and ask yourself these questions while you do:
- Is the QRS interval less than .09 seconds? Yes, it is within the normal range.
- Is the QRS complex wide or narrow? In this case, it's narrow.
- Are the QRS complexes similar in appearance or are there noticeable differences? In this case, we can see that each looks similar.
So, what is your cardiac interpretation? Based on these questions and on the findings from the ECG readout above, it would appear that this patient is in atrial fibrillation.
- We have an irregular rhythm.
- We have a rate that is 80 beats per minute but also irregular.
- The P-waves are missing.
- There is no PR interval.
- The QRS is less than .09 seconds and thus normal.
Pro Tip #2: Atrial fibrillation is rare in children. However, it can occur in pediatric patients with cardiomyopathy, and/or following complex heart surgery, and even more rarely in children with otherwise normal heart function.
For pediatric patients in atrial fibrillation, expert care and consultation is required to properly treat that child.
A Word About Survival Rates from Pediatric Cardiac Arrest
Survival rates from pediatric cardiac arrest vary according to the location of the arrest and the presenting rhythm.
According to the American Heart Association, the rate of survival to hospital discharge is higher if the arrest occurs in a hospital (43 percent) compared with out-of-hospital care (8 percent). Intact neurological survival is also greater if the cardiac arrest occurs while the patient is in a hospital.
It should be noted that the survival rate is higher (25 to 34 percent) when the patient's presenting rhythm is shockable (VF or pVT) compared to asystole (7 to 24 percent). The survival rate for a presenting rhythm of pulseless electrical activity is around 38 percent for in-hospital cardiac arrests.
However, when VF or pVT develop as a secondary rhythm during the resuscitation attempt for children in-hospital, survival rates are lower than those observed in cardiac arrests with non-shockable rhythms (11 percent vs. 27 percent, survival to discharge).
The highest survival rates (around 64 percent) occur when there is bradycardia and poor perfusion, and when chest compressions and ventilation are provided before pulseless arrest develops.




